We’re testing about 100 kids per day at our pediatric offices. Multiply that by all the pediatric offices in the Kansas City area. Add the testing done at our local hospital and testing centers. Add a few more tests done at home and school. And don’t forget about the pooled testing groups.
So. Many. Tests.
Even with this high volume, confusion remains about when to test and which to use. Since routine testing is an effective mitigation strategy, it’s important to get this right. Here’s your quick guide.
First, let’s talk about when to test.
When is determined by exposure history and symptoms. Generally speaking, most people need to be tested 5 days after any known exposure, regardless of vaccination status. In addition, testing is indicated when experiencing any new or significant illness symptoms. Students should receive guidance from their local school district regarding requirements for symptom testing. If not, this graphic may help.
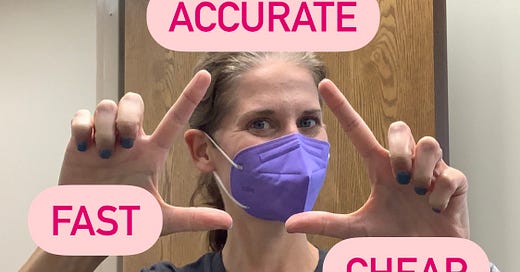
If testing is needed, there are two options, molecular (PCR) or antigen. Although both tests can be helpful, the information they provide is very different. Drop in the cost factor and you have a classic Iron Triangle.
When it comes to Covid testing, you can get it fast, accurate or cheap, but you can’t get it all.
In other words…
The most accurate test is cheap but not fast -- The “gold standard” PCR test.
A fast, cheap test is less accurate -- The rapid antigen test.
A fast and accurate test is not cheap -- The rapid PCR test.
The choice of Covid test depends on the purpose. To diagnose, choose a molecular test. To screen, choose an antigen test.
Molecular tests (PCR, RT-PCR) use amplification technology to find small amounts of viral genetic material. These tests are the most accurate to date, with the best results a few days after exposure or when you have symptoms. PCR testing is readily available in most communities across the US. In addition, some offices (including ours) have rapid PCR testing available. Rapid PCR provides nearly the same level of accuracy in less than an hour and is best used with symptomatic patients.
Use molecular tests for situations that need ACCURACY to determine if a person is infected. Molecular tests are the preferred test after any direct exposure history, when experiencing more than one Covid-like symptom, or if a child has illness symptoms and they (or someone they live with, like a pregnant person) are at high-risk of severe Covid-19 disease.
Molecular tests are preferred for situations like:
He’s had a direct exposure at school but has no symptoms. (Test 5 days after exposure. Out of quar on Day 7.)
I have a new cough but no known exposure.
She has a few mild symptoms and wants to get back to school.
I’ve had a direct exposure and feel fine, but I want to get out of self-quarantine early. (Test on Day 5. If negative, early release on Day 7.)
They’ve had an exposure, and they have a sore throat and headache.
I’ve recently traveled/been to an event and want to make sure I’m not infected.
He needs a pre-travel or pre-procedure test.
I might have been exposed to Covid a few days ago, but I’m feeling fine.
She’s going to visit her unvaccinated grandma this weekend. We want to be safe.
I’m pregnant, and my daughter woke up with a cough and runny nose.
In all situations where an antigen test may be used. (see below)
Friendly reminder: Until your test results return, you need to:
The other type of test is an antigen test (home tests and some school/doctor office tests.) These tests look for proteins on the viral surface and will only turn positive if you have significant symptoms (high viral load.) These tests are fairly accurate when a symptomatic person is positive, but a negative test cannot ensure that a person is healthy. Without symptoms, one rapid antigen test has very little value, but accuracy increases when tests are used in series (one test followed by a second test in 36 hours.) And these tests are used by some schools as part of the “test to stay/play” protocol.
Think of antigen tests as FAST and CHEAP “contagiousness” tests. A negative result suggests a person is not contagious with Covid virus at the moment the test was collected, but it cannot accurately determine if a person is infected.
Use antigen tests for situations like:
I was exposed last week and feel like crap this morning. (Positive suggests infection, but a negative result would need an additional PCR test.)
She woke up with only a runny nose and has not had any known exposures. (Repeat in 36 hours.)
He woke up with runny nose, fever and cough. (A positive would allow quick initiation of isolation plans, a negative still needs a PCR test.)
I’m on a sports team. We don’t wear masks during play, and I don’t want to expose my teammates. (Test to play protocol.)
She’s had a low-risk exposure and is feeling great. She wants to stay in school. (Test to stay protocol.)
School and workplace mitigation protocols.
Another reminder: After ANY positive Covid test, immediately isolate and consider yourself infected.
Obviously, this list is not exhaustive and families may have special situations in which better testing options exist. If you have questions, please reach out to your pediatrician’s office and we can help you make the best testing choice.
One final note: I know getting tested is not easy. It takes time, money and isn’t the most pleasant experience. So, I want to say thanks to all the parents who have been in the office to test their kids. Just like wearing masks and getting vaccinated, getting tested is an action that shows our children we are part of a community. And as community members, doing our best to stop the spread of infection is an effort that is worthy and right.
As we begin this school year, let’s continue to show grace and kindness to everyone doing their best. (Waving at all of my teachers out there! I see you.) We will make it through. Together.
Stay well,
Some other stuff:
It was my pleasure to talk about masks in school on NBC Nightly News: Kids Edition. In this episode, I demonstrate the “knot and tuck” technique to help surgical-type masks fit better on smaller faces.
If that isn’t enough, the most recent episode of #MasksOffLive Dr. Nicole and I talked about all things back-to-school, including masks and testing. Follow me on Insta to find out when the next #MasksOffLive will be lighting up.
Finally, I really liked this piece from Derek Thompson of The Atlantic. In it, he defends the end of “hygiene theater.” But keep washing your hands, okay?